The Opportunity: Improve the Quality of Care and Reduce Costs with Healthcare Data Analytics Services
Aetna, one of the nation’s largest insurers, partners with various Accountable Care Organizations (ACO) to deliver value-based care. Aetna wanted to help member ACOs better manage care delivery, reduce costs, and decrease the use of acute care services to improve patient outcomes.
Aetna understood that an Accountable Care Organization’s success is tied directly to quality data and analytics and using them to reduce the total cost of care for its patient population. Pivotal to this mission was a mechanism to facilitate care coordination and connect healthcare providers within an ACO.
Aetna sought to utilize MojoTech, a software development company with expertise in healthcare and analytics, to develop a custom solution while mentoring internal teams to optimize development and accelerate projects.
Our Response: Developing a HIPAA Compliant Analytics Solution using HL7 FHIR
The custom healthcare analytics solution aggregated data from multiple sources and created easy-to-use software to identify referral patterns and optimize network management.
Legacy Integration & Data Ingestion
Working with healthcare data is challenging as HIPAA regulations require privacy, security, and accuracy. Furthermore, data was resting in legacy systems, which needed to be integrated using HL7 FHIR. MojoTech used Ruby-on-Rails and PostgreSQL to create a flexible, robust data ingestion and transformation engine.
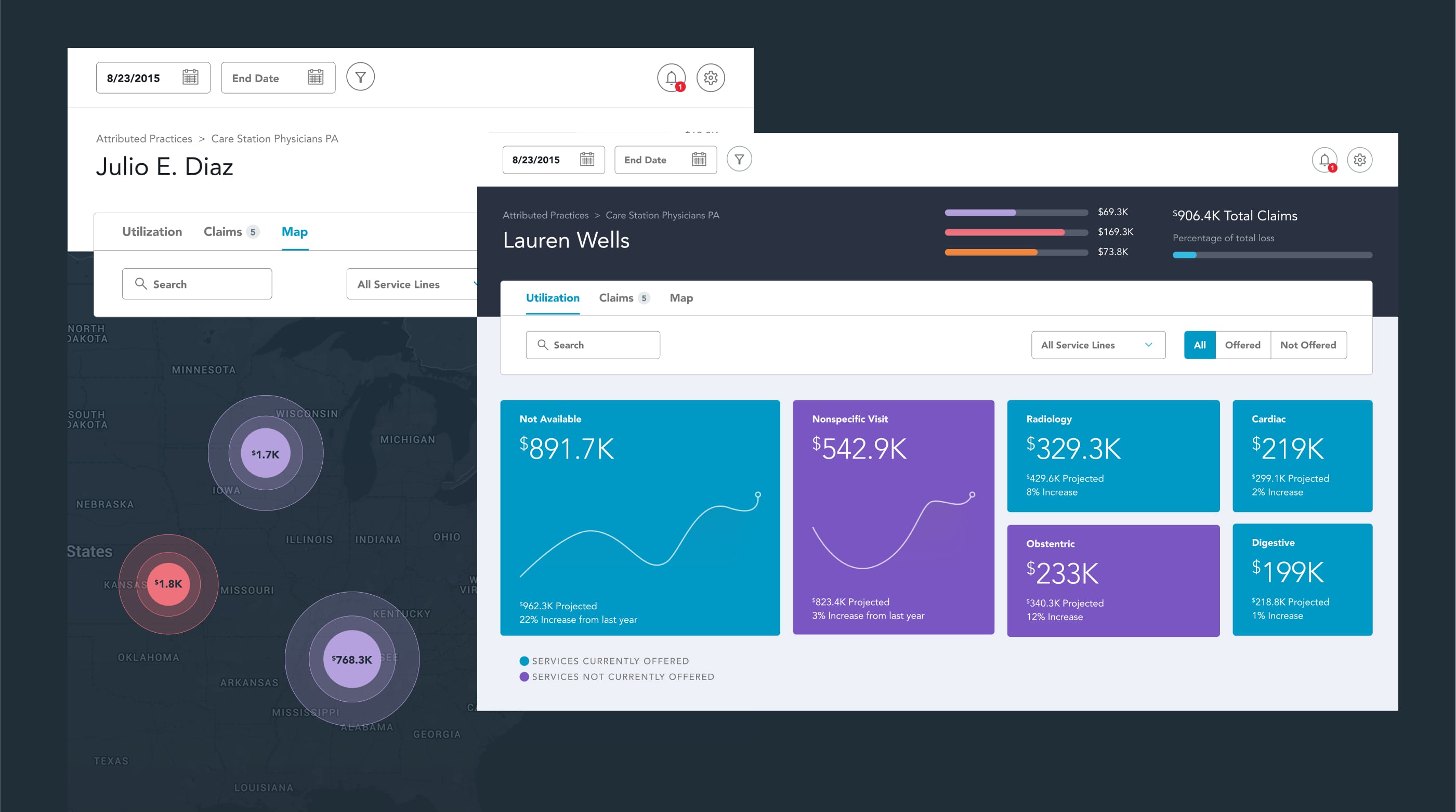
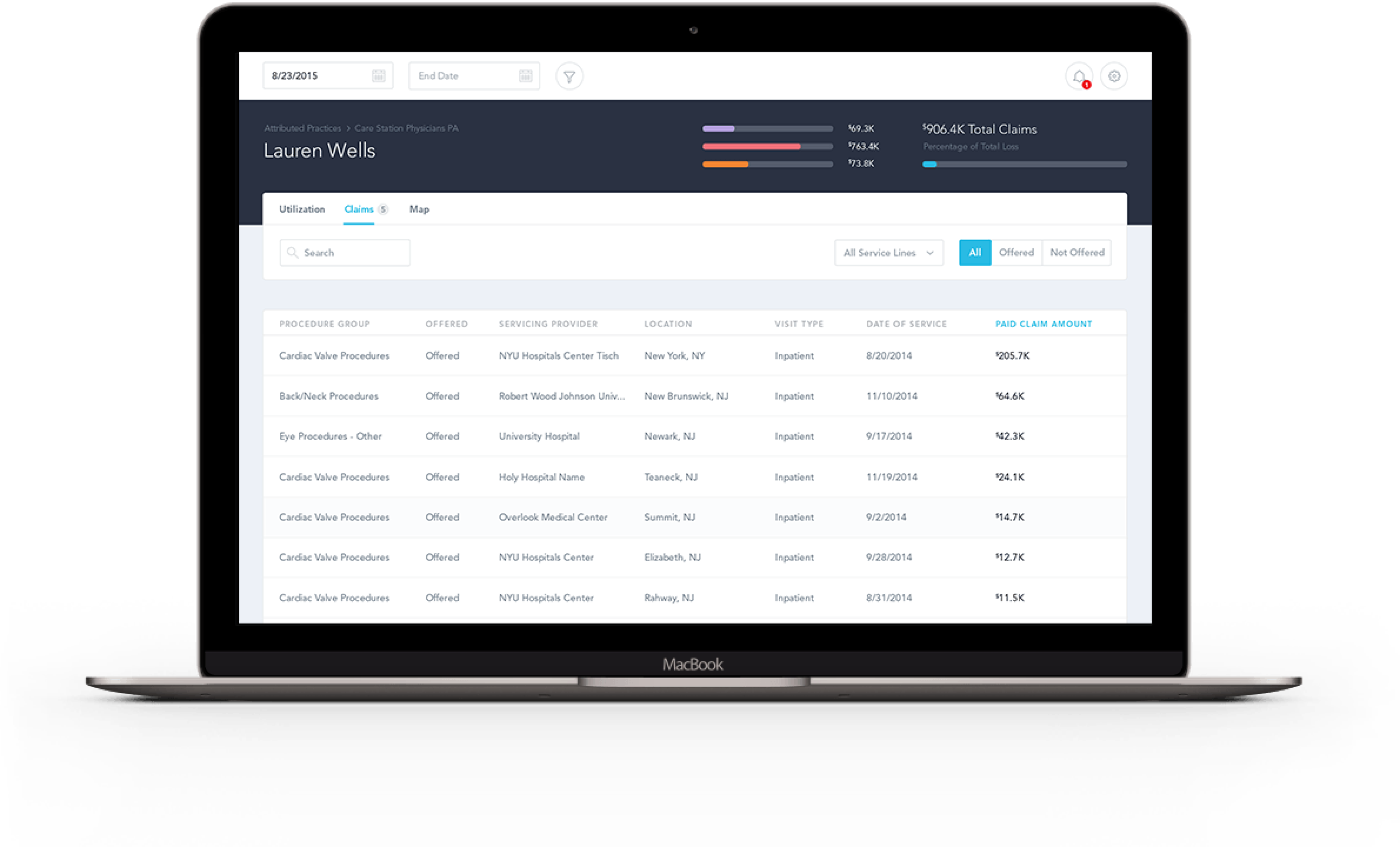
Data Visualization & UI/UX Design
The intuitive front end utilizes Angular, D3, and Google Maps to craft a User Interface that allows non-technical users to navigate and drill through complex data and obtain actionable, trackable insights.
Integrated test suites, including Cucumber and MiniTest with a Jenkins CI server, ensured quality code before deploying new features to a private cloud.
Product Management & Technology Mentoring
Often inside corporate tech teams with legacy products, the high cost of change dictates compartmentalization and stifles innovation. Aetna’s commitment to delivering real value to its customers came by embracing agile development processes that MojoTech has honed.
In this circumstance, the first step to success was implementing a project management and development practice that leveraged the strengths of both Aetna and MojoTech. Using a disciplined SCRUM approach, we seamlessly integrated the efforts of our developers, Aetna’s product owners, data suppliers, third-party design resources, and Aetna’s internal developers.
As a healthcare software development company, MojoTech has the luxury of constantly exploring new technologies and problem-solving approaches. We love working with our client’s internal technical teams, as we can share our best practices, mentor developers on the latest tools and frameworks, and, most importantly, ensure a smooth transition to in-house teams. We provide lifetime value to our clients beyond our engagements.
The Outcome: Data-driven Decisions Reduce Referral Leakage and Save Millions Throughout the Continuum of Care
Aetna and its ACO members utilized the custom healthcare analytics solution to gain valuable insights to improve the quality of care for its patients, reduce costs, and better manage the health of the population it serves.
Improved Patient Outcomes
By reducing patient leakage, Aetna and its ACO network improved patient outcomes by ensuring that patients receive comprehensive and coordinated care. As patients receive services from multiple providers, the analytics provides insights into their care and gives confidence that a patient's needs are met.
Cost Savings
Aetna helped its partner ACOs reduce costs by keeping patients within the network of providers. Patients receiving care from providers outside the ACO forces the ACO to spend more to acquire new patients. Additionally, patients insured by Aetna can save money by receiving better care from in-network providers, which reduces out-of-pocket expenses.